Purpose
This brief presents four case studies illustrating how primary care practices can effectively engage with their communities to support whole-person care. Each case study highlights the need identified in the practice or community and the community-based intervention conducted in response, as well as the funding sources, results, and key takeaways. The case studies offer diverse approaches and strategies that primary care teams can use to engage with their communities to address health-related social needs (HRSN) and improve health outcomes. The four case studies include:
- The CUNA Program, Cherokee Health Systems and Centro Hispano de East Tennessee
- Vietnamese Family Autism Advisory Board, HopeCentral Clinic
- Supporting Families Growing Together Initiative, MaineHealth System
- Opioid Centers of Excellence Model, Pennsylvania Department of Human Services
Definitions
Whole-person care (also referred to as whole health care) is a team-based, person-centered approach that considers the behavioral, environmental, social, and other factors that influence health outcomes and move people toward chronic disease.1,2 This approach is anchored in trusted, longitudinal relationships. It involves tailoring and delivering care to align with the needs, goals, and cultural and linguistic preferences of people, families, and communities.3 No one primary care clinician or practice has the capacity to perform all the functions required to achieve whole-person care.4 Whole-person care requires integrated, collaborative, interdisciplinary care teams to share responsibilities and coordinate patient care.5
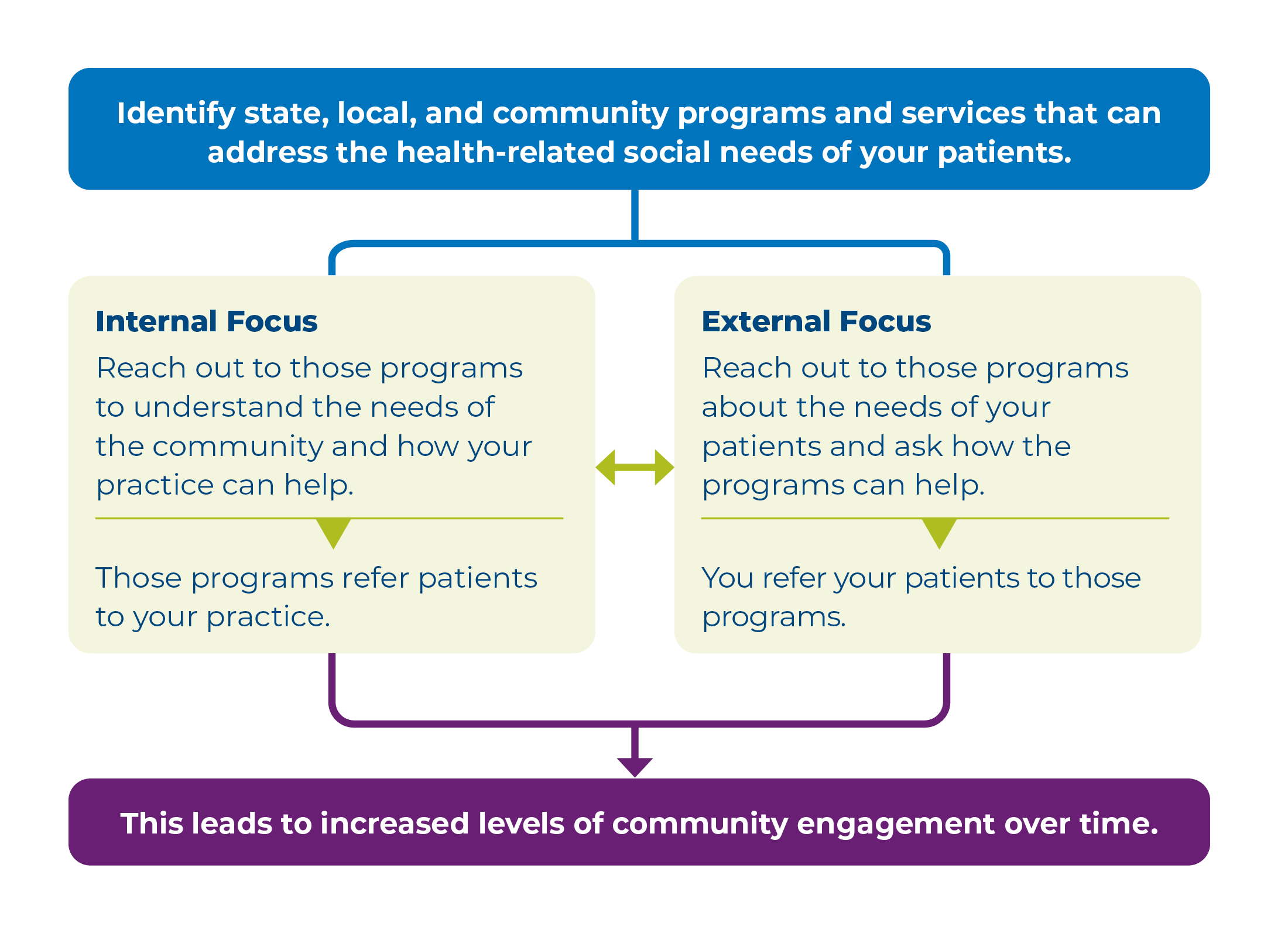
Community engagement is "the process of working collaboratively with and through groups of people affiliated by geographic proximity, special interest, or similar situations to address issues affecting the wellbeing of those people".6 Community engagement requires ongoing collaboration with community members and organizations to address their health needs and health-related social needs. For primary care practices, this involves proactively building trusting relationships with local providers, agencies, and organizations to facilitate access to healthcare, health education, health data, and social services and supports.7
1. Hernandez R, Bassett SM, Boughton SW, Schuette SA, Shiu EW, Moskowitz JT. Psychological well-being and physical health: associations, mechanisms, and future directions. Emot Rev. 2018 Jan;10(1):18-29. https://doi.org/10.1177/1754073917697824. Accessed July 5, 2024.
2. Thomas H, Mitchell G, Rich J, Best M. Definition of whole person care in general practice in the English language literature: a systematic review. BMJ open. 2018 Dec 1;8(12):e023758. https://doi.org/10.1136/bmjopen-2018-023758. Accessed September 3, 2024.
3. National Center for Complementary and Integrative Health. Whole Person Health: What You Need To Know. https://www.nccih.nih.gov/health/whole-person-health-what-you-need-to-know. Accessed July 5, 2024.
4. National Academies of Sciences, Engineering, and Medicine. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. Washington, DC: The National Academies Press; 2021. https://doi.org/10.17226/25983. Accessed July 5, 2024.
5. National Academies of Sciences, Engineering, and Medicine. Defining whole health. In: Achieving Whole Health: A New Approach for Veterans and the Nation. Washington, DC: The National Academies Press; 2023: chapter 2. https://doi.org/10.17226/26854. Accessed July 5, 2024.
6. Clinical and Translational Science Awards Consortium, Community Engagement Key Function Committee. Chapter 1. community engagement: definitions and organizing concepts from the literature. In: Principles of Community Engagement. 2nd ed. Atlanta, GA: Agency for Toxic Substances and Disease Registry, Centers for Disease Control and Prevention; 2011. https://stacks.cdc.gov/view/cdc/11699. Accessed July 5, 2024.
7. Erku D, Khatri R, Endalamaw A, Wolka E, Nigatu F, Zewdie A, Assefa Y. Community engagement initiatives in primary health care to achieve universal health coverage: A realist synthesis of scoping review. Plos one. 2023 May 3;18(5):e0285222. https://doi.org/10.1371%2Fjournal.pone.0285222. Accessed September 4, 2024.
8. Gunja MZ, Gumas ED, Williams II RD. U.S. Health Care from a Global Perspective, 2022: Accelerating Spending, Worsening Outcomes. New York, NY: Commonwealth Fund; January 2023. https://doi.org/10.26099/8ejy-yc74. Accessed July 5, 2024.
9. Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, Lee A, Khan AR, Ahmadi A, Ferrari AJ, Kasaeian A. The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US states. Jama. 2018 Apr 10;319(14):1444-72. https://jamanetwork.com/journals/jama/fullarticle/2678018. Accessed September 3, 2024.
10. Buttorff C, Ruder T, Bauman M. Multiple Chronic Conditions in the United States. Arlington, VA: RAND Corporation; 2017. https://www.rand.org/pubs/tools/TL221.html. Accessed September 3, 2024.
11. Walker ER, Druss BG. Cumulative burden of comorbid mental disorders, substance use disorders, chronic medical conditions, and poverty on health among adults in the USA. Psychology, health & medicine. 2017 Jul 3;22(6):727-35. https://doi.org/10.1080/13548506.2016.1227855. Accessed September 2, 2024.
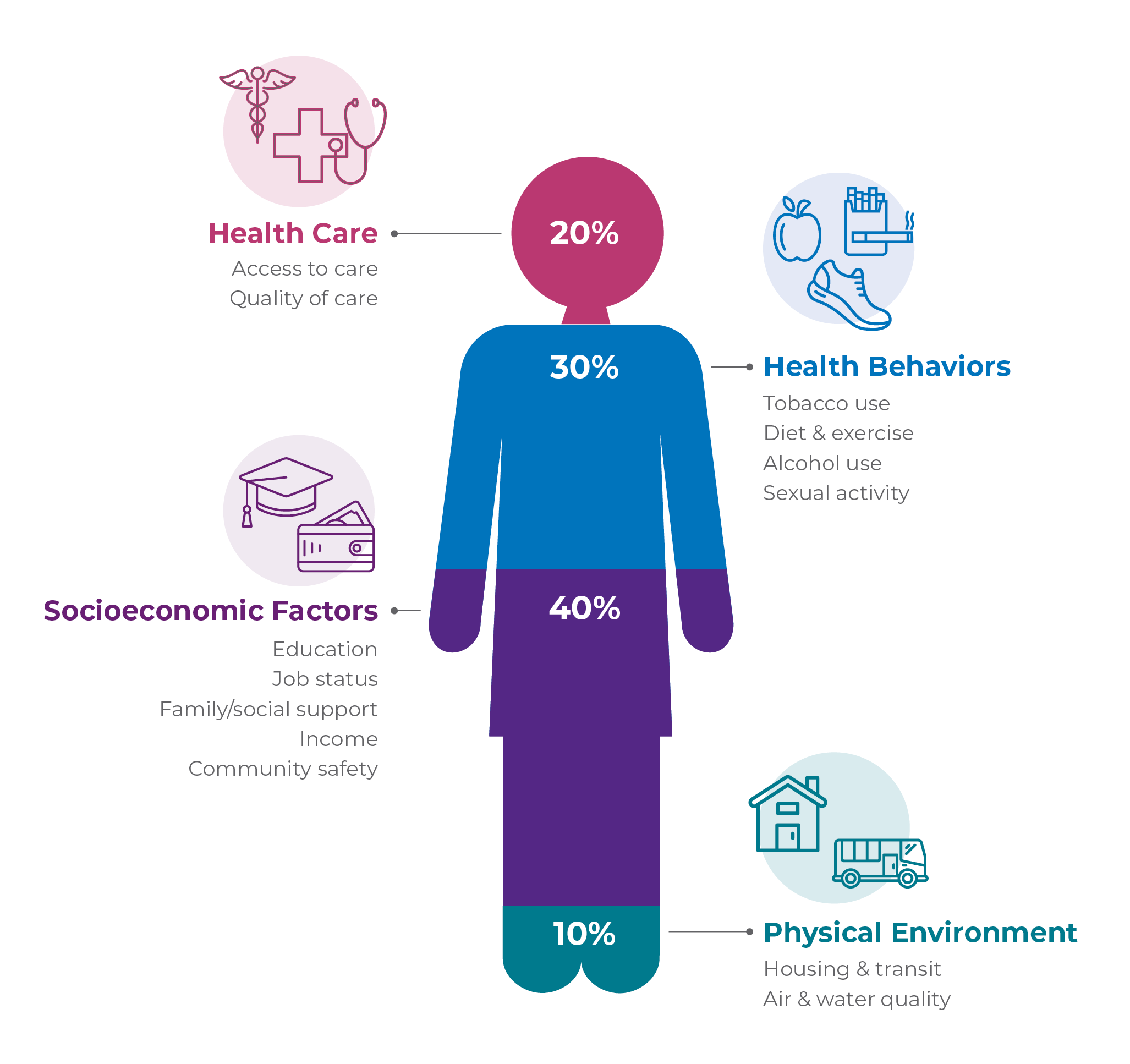
12. County Health Rankings and Roadmaps. County Health Rankings' Model of Health. https://www.countyhealthrankings.org/what-impacts-health/county-health-rankings-model. Accessed July 5, 2024.
13. Office of the Assistant Secretary for Planning and Evaluation. HHS Call to Action: Addressing Health-Related Social Needs in Communities Across the Nation. Washington, DC: U.S. Department of Health and Human Services; November 2023. https://aspe.hhs.gov/sites/default/files/documents/3e2f6140d0087435cc6832bf8cf32618/hhs-call-to-action-health-related-social-needs.pdf (PDF - 875 KB). Accessed July 5, 2024.
14. County Health Rankings and Roadmaps. County Health Rankings' Model of Health. https://www.countyhealthrankings.org/what-impacts-health/county-health-rankings-model. Accessed July 5, 2024.
15. Office of the Assistant Secretary for Planning and Evaluation. HHS Call to Action: Addressing Health-Related Social Needs in Communities Across the Nation. Washington, DC: U.S. Department of Health and Human Services; November 2023. https://aspe.hhs.gov/sites/default/files/documents/3e2f6140d0087435cc6832bf8cf32618/hhs-call-to-action-health-related-social-needs.pdf (PDF - 875 KB). Accessed July 5, 2024.
16. Kreuter MW, Thompson T, McQueen A, Garg R. Addressing social needs in health care settings: evidence, challenges, and opportunities for public health. Annual review of public health. 2021 Apr 1;42(2021):329-44. https://doi.org/10.1146%2Fannurev-publhealth-090419-102204. Accessed September 5, 2024.
17. National Academies of Sciences, Engineering, and Medicine. Defining whole health. In: Achieving Whole Health: A New Approach for Veterans and the Nation. Washington, DC: The National Academies Press; 2023: chapter 2. https://doi.org/10.17226/26854. Accessed July 5, 2024.
18. Meyers DJ, Chien AT, Nguyen KH, Li Z, Singer SJ, Rosenthal MB. Association of team-based primary care with health care utilization and costs among chronically ill patients. JAMA Internal Medicine. 2019 Jan 1;179(1):54-61. https://doi.org/10.1001/jamainternmed.2018.5118. Accessed July 5, 2024.
19. Dai M, Willard-Grace R, Knox M, Larson SA, Magill MK, Grumbach K, Peterson LE. Team configurations, efficiency, and family physician burnout. The Journal of the American Board of Family Medicine. 2020 May 1;33(3):368-77. https://doi.org/10.3122/jabfm.2020.03.190336. Accessed July 5, 2024.
20. Kong M, Bodenheimer T. Primary care urgently needs support for interprofessional teams. The Permanente Journal. 2022;26(4):100. https://doi.org/10.7812%2FTPP%2F22.105. Accessed July 5, 2024.
21. Office of the Assistant Secretary for Planning and Evaluation. HHS Call to Action: Addressing Health-Related Social Needs in Communities Across the Nation. Washington, DC: U.S. Department of Health and Human Services; November 2023. https://aspe.hhs.gov/sites/default/files/documents/3e2f6140d0087435cc6832bf8cf32618/hhs-call-to-action-health-related-social-needs.pdf (PDF - 875 KB). Accessed July 5, 2024.
22. Benavidez GA, Zahnd WE, Hung P, Eberth JM. Chronic disease prevalence in the us: sociodemographic and geographic variations by zip code tabulation area. Prev Chronic Dis. 2024;21:230267. https://dx.doi.org/10.5888/pcd21.230267. Accessed July 5, 2024.
23. National Academies of Sciences, Engineering, and Medicine. Whole health systems' Evidence. In: Achieving Whole Health: A New Approach for Veterans and the Nation. Washington, DC: The National Academies Press; 2023: chapter 5. https://doi.org/10.17226/26854. Accessed September 4, 2024.
24. Counsell SR, Callahan CM, Clark DO, Tu W, Buttar AB, Stump TE, Ricketts GD. Geriatric care management for low-income seniors: a randomized controlled trial. Jama. 2007 Dec 12;298(22):2623-33. https://doi.org/10.1001/jama.298.22.2623. Accessed September 3, 2024.
25. Bokhour BG, Hyde J, Kligler B, Gelman H, Gaj L, Barker AM, Douglas J, DeFaccio R, Taylor SL, Zeliadt SB. From patient outcomes to system change: Evaluating the impact of VHA's implementation of the Whole Health System of Care. Health services research. 2022 Jun;57:53-65. https://doi.org/10.1111/1475-6773.13938. Accessed September 3, 2024.
26. Sinaii N. Mary's Center's Social Change Model Quantitative Research Study. (Presented at Mary's Center Symposium on October 12, 2018.) Washington, DC: Mary's Center; 2018. Accessed September 4, 2024.
27. Blash L, Dower C, Chapman S. Southcentral Foundation—Nuka Model Of Care Provides Career Growth For Frontline Staff. Research Brief. San Francisco, CA: Center for the Health Professions at UCSF; January 2012. https://healthforce.ucsf.edu/sites/healthforce.ucsf.edu/files/publication-pdf/2011_09_Southcentral_Foundation-Nuka_Model_of_Care_Provides_Career_Growth_for_Frontline_Staff.pdf (PDF - 172 KB). Accessed September 3, 2024.
28. Jones C, Finison K, McGraves-Lloyd K, Tremblay T, Mohlman MK, Tanzman B, Hazard M, Maier S, Samuelson J. Vermont's community-oriented all-payer medical home model reduces expenditures and utilization while delivering high-quality care. Population health management. 2016 Jun 1;19(3):196-205. https://doi.org/10.1089/pop.2015.0055. Accessed September 4, 2024.
29. National Academies of Sciences, Engineering, and Medicine. Defining whole health. In: Achieving Whole Health: A New Approach for Veterans and the Nation. Washington, DC: The National Academies Press; 2023: chapter 2. https://doi.org/10.17226/26854. Accessed July 5, 2024.
30. Erku D, Khatri R, Endalamaw A, Wolka E, Nigatu F, Zewdie A, Assefa Y. Community engagement initiatives in primary health care to achieve universal health coverage: A realist synthesis of scoping review. Plos one. 2023 May 3;18(5):e0285222. https://doi.org/10.1371%2Fjournal.pone.0285222. Accessed September 4, 2024.
31. National Academies of Sciences, Engineering, and Medicine. Defining whole health. In: Achieving Whole Health: A New Approach for Veterans and the Nation. Washington, DC: The National Academies Press; 2023: chapter 2. https://doi.org/10.17226/26854. Accessed July 5, 2024.
32. National Academies of Sciences, Engineering, and Medicine. Defining whole health. In: Achieving Whole Health: A New Approach for Veterans and the Nation. Washington, DC: The National Academies Press; 2023: chapter 2. https://doi.org/10.17226/26854. Accessed July 5, 2024.
33. Erku D, Khatri R, Endalamaw A, Wolka E, Nigatu F, Zewdie A, Assefa Y. Community engagement initiatives in primary health care to achieve universal health coverage: A realist synthesis of scoping review. Plos one. 2023 May 3;18(5):e0285222. https://doi.org/10.1371%2Fjournal.pone.0285222. Accessed September 4, 2024.
34. Centro Hispano de East TN. Hispanic Heritage Month: Family & Maternal Health. https://www.centrohispanotn.org/2023/09/hispanic-heritage-month-family-maternal-health/. Accessed July 5, 2024.
35. Fryer K, Lewis G, Munoz C, Stuebe AM. Identifying barriers and facilitators to prenatal care for Spanish-speaking women. N C Med J. 2021 Jan-Feb;82(1):7-13. www.doi.org/10.18043/ncm.82.1.7. Accessed September 4, 2024.
36. Hoyert DL. Maternal Mortality Rates in the United States, 2021. https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2021/maternal-mortality-rates-2021.htm. Accessed July 5, 2024.
37. United States Government Accountability Office. Maternal Health: Outcomes Worsened and Disparities Persisted During the Pandemic. GAO-23-105871. Washington, DC: United States Government Accountability Office; October 2022. https://www.gao.gov/assets/gao-23-105871.pdf (PDF - 541 KB). Accessed July 5, 2024.
38. Funk C, Lopez MH. 2. Hispanic Americans' experiences with health care. In: Hispanic Americans' Trust in and Engagement With Science. Washington, DC: Pew Research Center; June 2022. https://www.pewresearch.org/science/2022/06/14/hispanic-americans-experiences-with-health-care/. Accessed July 5, 2024.
39. Vietnamese Family Autism Advisory Board. Homepage. https://vfaab.org/. Accessed July 5, 2024.
40. Centers for Disease Control and Prevention. Autism Spectrum Disorder (ASD): Data and Statistics on Autism Spectrum Disorder. https://www.cdc.gov/autism/data-research/index.html. Accessed September 4, 2024.
41. Okoye C, Obialo-Ibeawuchi CM, Obajeun OA, Sarwar S, Tawfik C, Waleed MS, Wasim AU, Mohamoud I, Afolayan AY, Mbaezue RN. Early diagnosis of autism spectrum disorder: a review and analysis of the risks and benefits. Cureus. 2023 Aug 9;15(8):e43226. https://www.doi.org/10.7759/cureus.43226. Accessed September 4, 2024.
42. Bivarchi FA, Kehyayan V, Al-Kohji SM. Barriers to the early detection and intervention of children with autism spectrum disorders: A literature. Journal of Nursing Education and Practice. 2021;11(11):72-80. https://www.sciedu.ca/journal/index.php/jnep/article/viewFile/20301/12792 (PDF - 209 KB). Accessed September 4, 2024.
43. Huda E, Hawker P, Cibralic S, John JR, Hussain A, Diaz AM, Eapen V. Screening tools for autism in culturally and linguistically diverse paediatric populations: a systematic review. Research Square. 2023. https://doi.org/10.21203/rs.3.rs-3669264/v1. Accessed September 4, 2024.
44. John T. Gorman Foundation. Featured Initiatives. https://www.jtgfoundation.org/our-work/featured-initiatives/. Accessed July 5, 2024.
45. Metzler M, Merrick MT, Klevens J, Ports KA, Ford DC. Adverse childhood experiences and life opportunities: shifting the narrative. Children and Youth Services Review. 2017 Jan 1;72:141-9. https://doi.org/10.1016/j.childyouth.2016.10.021. Accessed July 5, 2024.
46. Moore TG, McDonald M, Carlon L, O'Rourke K. Early childhood development and the social determinants of health inequities. Health Promotion International. 2015 Sep 1;30(suppl_2):ii102-15. https://doi.org/10.1093/heapro/dav031. Accessed July 5, 2024.
47. The Center on the Developing Child. Brain Architecture. https://developingchild.harvard.edu/science/key-concepts/brain-architecture/. Accessed July 5, 2024.
48. Maggi S, Irwin LJ, Siddiqi A, Hertzman C. The social determinants of early child development: an overview. Journal of Pediatrics and child health. 2010 Nov;46(11):627-35. https://doi.org/10.1111/j.1440-1754.2010.01817.x. Accessed July 22, 2024.
49. National Scientific Council on the Developing Child. Excessive stress disrupts the architecture of the developing brain. Working Paper No. 2005 Oct 12;3. https://developingchild.harvard.edu/wp-content/uploads/2024/10/Stress_Disrupts_Architecture_Developing_Brain-1.pdf (PDF - 506 KB). Accessed July 22, 2024.
50. Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, and Section on Developmental and Behavioral Pediatrics, Garner AS, Shonkoff JP, Siegel BS, Dobbins MI, Earls MF, Garner AS, McGuinn L, Pascoe J, Wood DL. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012 Jan 1;129(1):e224-31. https://doi.org/10.1542/peds.2011-2662. Accessed July 5, 2024.
51. Commonwealth of Pennsylvania. Centers of Excellence. https://www.pa.gov/en/agencies/dhs/resources/mental-health-substance-use-disorder/substance-use-disorder/centers-of-excellence.html. Accessed July 5, 2024.
52. Spencer MR, Garnett MF, Miniño AM. Drug overdose deaths in the United States, 2002–2022. NCHS Data Brief, no 491. Hyattsville, MD: National Center for Health Statistics. 2024. https://dx.doi.org/10.15620/cdc:135849. Accessed September 4, 2024.
53. Pennsylvania Office of Attorney General. Opioid Battle. https://www.attorneygeneral.gov/protect-yourself/opioid-battle. Accessed September 4, 2024.
54. Lagisetty P, Klasa K, Bush C, Heisler M, Chopra V, Bohnert A. Primary care models for treating opioid use disorders: What actually works? A systematic review. PloS one. 2017 Oct 17;12(10):e0186315. https://doi.org/10.1371/journal.pone.0186315. Accessed September 4, 2024.
55. Buresh M, Stern R, Rastegar D. Treatment of opioid use disorder in primary care. bmj. 2021 May 19;373. https://doi.org/10.1136/bmj.n784. Accessed September 4, 2024.
56. Alaigh P, Zander G, Pringle JL. Pennsylvania's novel public-private approach to combatting the opioid crisis. NEJM Catalyst Innovations In Care Delivery. 2020 Oct 1;1(5). https://catalyst.nejm.org/doi/abs/10.1056/CAT.20.0302. Accessed July 5, 2024.
57. America Counts Staff. Pennsylvania Population Hit 13 Million in 2020. https://www.census.gov/library/stories/state-by-state/pennsylvania.html. Accessed July 5, 2024.